Cure4CF Update
“The number” – the changing landscape of lung function testing in cystic fibrosis
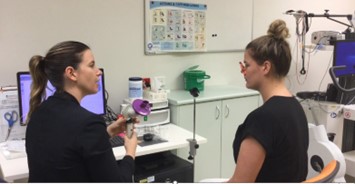
When we visited the Mater in Brisbane last year as part of our tour with Dr Lucy Burr we visited the lung function laboratory. Here we met Respiratory Scientist Grace Madden who talked to us about the changing landscape of lung function assessment in cystic fibrosis. Keen to learn more, I caught up with Grace recently to talk about the changing landscape of lung function assessment for cystic fibrosis.
What is Lung Function Testing?
Lung function testing is the first part of the clinic process at the Mater. Lung or pulmonary function tests are most often performed in a specialised and accredited laboratory. They are used to measure how your lungs are working. Spirometry is probably the most used test which measures how much are you can breathe into your lungs and how fast you can blow the air from your lungs. After taking a big breath in, the team will ask you to blow that breath out as hard and fast as you possibly can.
This can take a lot of effort and can be really tiring for people with CF. The result most people are familiar with is the FEV1 – which stands for the Forced Expiratory Volume in 1 second, where forced expiratory means – how hard and fast you breath out and the volume in 1 second is the amount of air that was expired in the first second. This number is usually expressed as a percentage and is compared to a reference range so the team can see how your lung function compares to others the same age, gender, race and height. It’s important to remember that everyone’s lungs are different shapes and sizes, and normal results differ from person to person. Because of this, the team will often look at your own results over time, as this helps indicate how your lungs are doing compared to your baseline.
https://www.cfwa.org.au/wp-content/uploads/2021/12/Spirometry-2021.pdf is a great resource on spirometry from CF WA if you would like to know more.
Why do I have to repeat the test so many times?
If you have done a spirometry test, you might recall having to repeat the test a few times. This is important because the result is impacted by how the person has performed the test and if they have coughed while breathing out, or they might not have been sitting up as straight as possible – which many have prevented them taking the biggest breath in possible. There are lots of reasons your team might as you do to the test again. The international standards recommend at least 3 efforts. Quite often, your lungs need to warm up, so your first attempt may not be the best result of the day.
Grace explained that the pressure to get the best number could sometimes result in the person or their family wanting to do more attempts. Having an experienced respiratory scientist to support the person and their family to understand the results is important. Often because more attempts do not result in a better number – because the test is dependent on effort, it can be really tiring to do the test repeatedly and result in the person not being able to achieve their best result.

How has the importance of “the number” changed?
Grace explained that people in the clinic understand that when they do their lung function testing, if a low number was produced, this meant they had to cancel their plans and might likely be admitted to hospital. Low numbers usually meant infections or some other issue that required hospitalisation to rapidly receive treatment. This meant that young people were often anxious about “the number” and of course, their families were also often anxious and worried, eagerly awaiting the result.
Advancements in CF care in terms of infection control and mucus management and now with modulator therapy being accessible for many people with CF have meant that for Grace and her team, spirometry is now easier and quicker to undertake. People are feeling better and experience less coughing and are becoming less focussed on “the number”. Now the focus is more about the change in the number between clinic visits, has it changed from last clinic. If the change was a reduction in lung function, then the team will look at how big the change is and use other assessments to understand what has resulted in this change. Small changes are often nothing to worry about and can be part of the normal variation.
My lung function is “normal”, what does this mean for my lung health?
For many young people with CF now, lung function is often in the healthy range or “normal”. While this is a life changing improvement it does offer some challenges for CF teams. Grace and her team at the Mater are exploring new ways to be able to assess lung function and changes in lung health in this new era of normal lung function. Some of the new techniques include the Lung Clearance Index (LCI) and Forced Oscillation Technique (FOT).
About the Lung Clearance Index
The lung clearance index (LCI) scores how well air moves though the lungs. It is very sensitive non-invasive and safe test that can detect early lung changes. It is measured by multiple breath nitrogen washout. Other than being able to pick up early changes in the lungs that may not be detectable by regular spirometry, this technique does not require a forced breath like FEV1 and reduces the effort needed for the person with CF. The other advantage of this technique is that it can be done easily with preschool age children who can enjoy a video while they are doing the test. This means it can easily be assessed during exacerbations as well during times of wellness. The person breathes in a tracer gas – often 80% nitrogen – and then breathes in 100% oxygen to wash the nitrogen out. Nitrogen is the most abundant gas in the atmosphere and completely safe to inhale. The regular air we breathe every day is 78% nitrogen.
About Grace
Grace has a Master of Clinical Science in sleep, respiratory and cardiovascular medicine. She started her career working nights in the sleep laboratory supervising and supporting people undertaking their sleep studies. In time she moved into the respiratory laboratory and has a passion for supporting young people with CF and their families. She is the current President of the Australian and New Zealand Society of Respiratory Science, which is an international body of scientists and technologist in respiratory function laboratories.
References
Lombardi, E., Gambazza, S., Pradal, U. et al. Lung clearance index in subjects with cystic fibrosis in Italy. Ital J Pediatr 45, 56 (2019). https://doi.org/10.1186/s13052-019-0647-5